Non-Small Cell Lung Cancer At Phoebe Putney Memorial Hospital
Lung cancer remains the leading cause of cancer death in the United States with nearly 156,000 deaths annually, accounting for approximately 25% of all cancer-related deaths. In the state of Georgia, it accounts for over 6,600 deaths each year. Both the incidence of lung cancer and mortality associated with it have been declining since the mid-1990’s, however, both are declining more rapidly in men than in women.
The development of lung cancer is strongly associated with cigarette smoking and to a lesser extent with exposure to radon, secondhand smoke, asbestos and numerous other environmental factors. The decreasing incidence of this cancer is primarily due to the decreasing rates of smoking that are taking place. The decreasing smoking rates are a result of a number of efforts including increased taxation on tobacco products, restrictions on advertising, warnings on cigarette packaging and general negative publicity.
Lung cancer is generally divided into two primary types, small cell lung cancer and non-small cell lung cancer (NSCLC) making up approximately 15% and 85% of all lung cancers respectively. Non-small cell lung cancers have traditionally been further divided into two major types, adenocarcinoma and squamous cell carcinoma with a small number of other relatively rare subtypes. Through numerous scientific advances, other factors have been identified such as epidermal growth factor receptors (EGFR) and anaplastic lymphoma kinase (ALK) that are expressed by some tumors and for which targeted therapies are available.
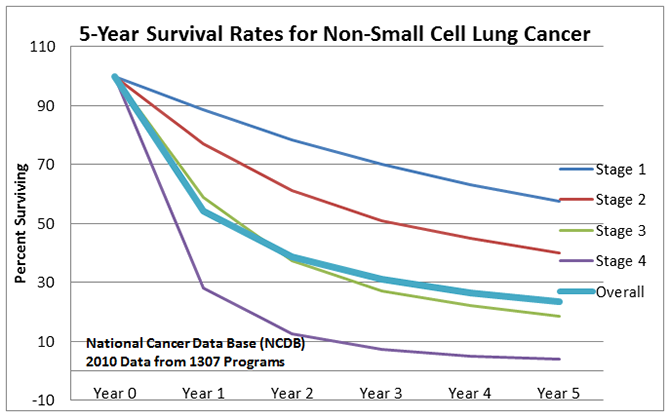
As with most cancers, detection at an earlier stage, when the cancer is smaller and has not spread, leads to improved overall survival. The overall 5-year survival for NSCLC is less than 25%. For stage I, it is nearly 60% while the 5 year survival for stage IV (metastatic) NSCLC is less than 5%. Data from the National Cancer Data Base (NCDB) on 5-year survival clearly shows this advantage of diagnosing at an earlier stage.
Through the early 2000s clinical trials were conducted using low dose spiral CT (LDCT) scans to evaluate effectiveness as a screening tool for identifying early stage lung cancers. In general, those studies were positive for subsets of patients who were identified as high risk.
In anticipation of this important screening tool becoming approved for generalized use in high risk patients, in January of 2014 Phoebe launched the LungWatch program. This program established primary care and family practice physicians as the gateway into the program, provided smoking cessation services, and, because it was not yet approved by Medicare or the major insurers, the scans were provided free to those patients who were eligible, based on risk, within the Phoebe primary service area. The U.S Preventive Services Task Force recommended LDCT as an appropriate screening modality and, in February of 2016, Medicare agreed that they would pay for this screening.
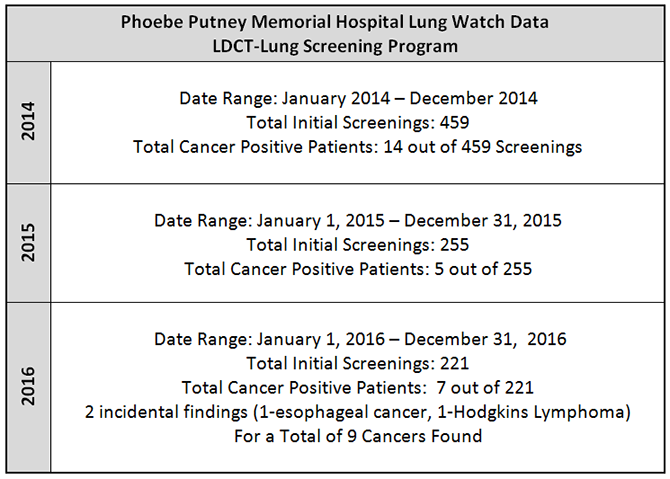
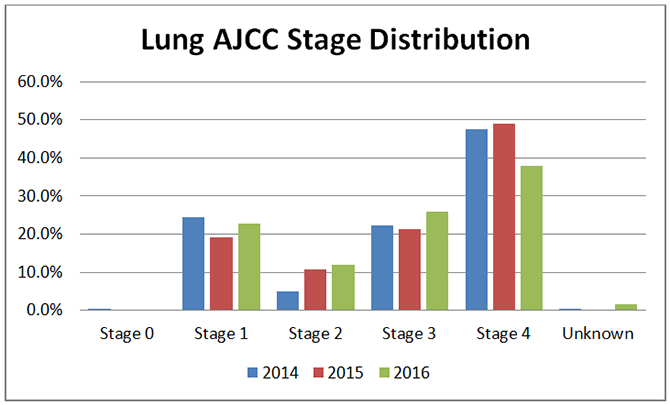
The Phoebe LungWatch program is now recognized as a Lung Cancer Screening Center of Excellence by the Lung Cancer Alliance. The program is staffed with two RN Lung Navigators and, screens an average of over 350 high risk patients each year and diagnoses an average of 10 lung cancers each year of which 80% are considered early stage and thus much more likely to be cured. Primarily as a result of this program Phoebe has seen its rate of Stage I and II NSCLC increase from 29% to 34% and its rate of stage IV NSCLCs drop from 47% to 38% of all NSCLC cases. Nationally, approximately 50% of lung cancers are diagnosed as Stage IV.
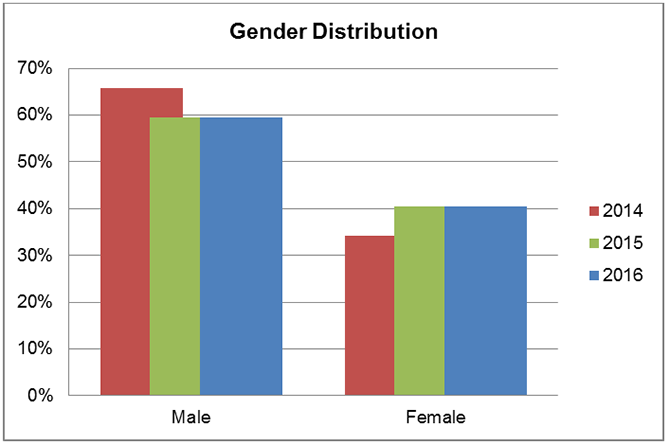
Data from the Phoebe Tumor Registry shows that the ratio between males and females differs from national data where 53% are males and 47% are females. At Phoebe 59% are males and only 41% are females. It is unclear what accounts for this observed difference.
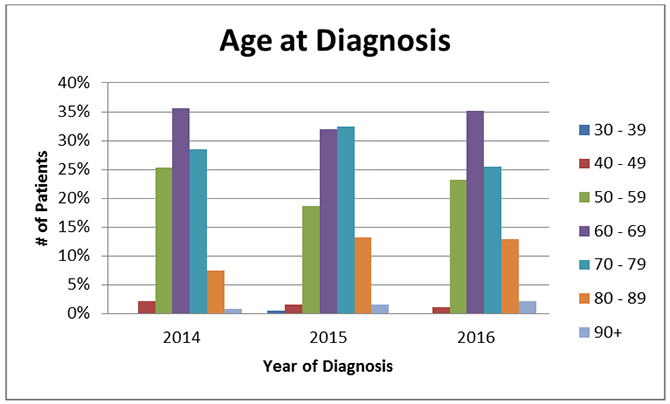
Like many cancers, lung cancer is also associated with increased age. 75% of cases are diagnosed in individuals 60 or older. The percentages by decade have remained relatively stable over the three years being reported.
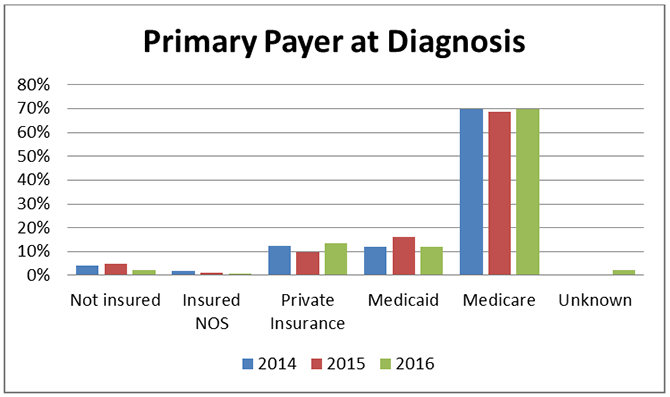
Because of this prevalence among older patients, a vast majority of the patients have Medicare for their medical coverage.
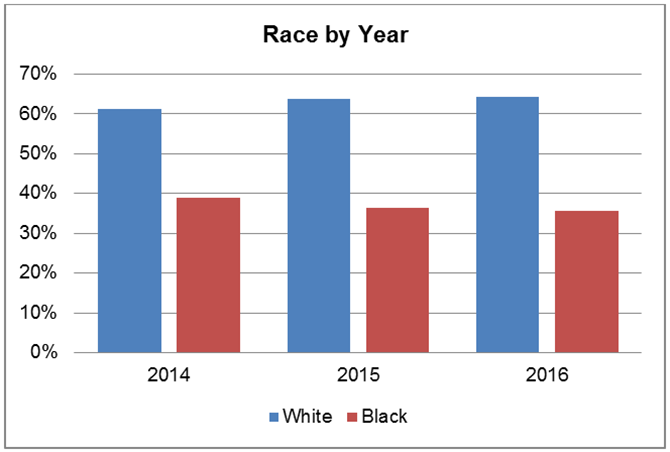
In Georgia, smoking prevalence is highest among non-Hispanic (NH) whites at 24% or 1 million individuals followed by NH blacks at 17% or 350,000 individuals. The high correlation between smoking and the development of lung cancer is reflected in the percentage of incidence per year by race where there are nearly two times as many cases diagnosed in whites as there are among blacks.
The gold standard for the quality of cancer care is the measurement of 5-year survival, the percentage of patients alive 5 years after diagnosis. Based on 2011 data (to allow 5 years of follow-up) Phoebe appears to fall below the U.S. statistics from the National Cancer Data Base (NCDB) for overall (all stages combined) with 11% survival versus 24%.
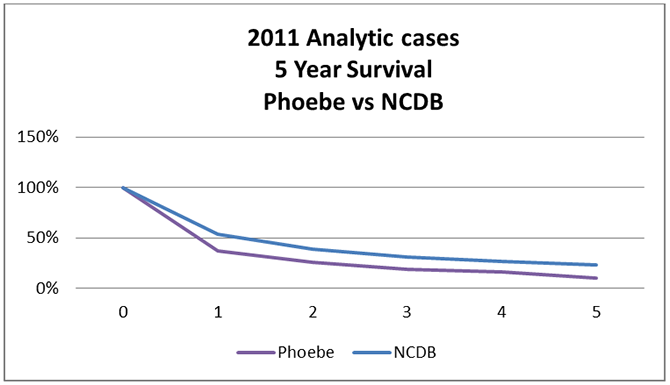
Because the 2011 cases predated the development of the LungWatch program and with significantly fewer Stage IV cases now being diagnosed at Phoebe when compared to national numbers, it is expected that 5-year survival will soon be very comparable, if not better than national numbers. Advances in genomic testing and the development of treatments targeted at these genomic findings will provide further advantage to the lung cancer patients of this region. That may or may not be partially offset by transportation and a financial issue that present in our generally rural area with it’s higher than normal levels of poverty. Continuing the lung screening program and addressing the social issues of our region provide the best chances of making progress against this very deadly disease.
Bibliography:
Cancer Facts and Figures 2017. American Cancer Society. Available online: https://www.cancer.org/.../cancer-facts-statistics/...cancer-facts-figures/cancer-facts-fig.
Disparities in Tobacco Use in Georgia. The Georgia Department of Public Health. Available online: http://ecphd.com/wp-content/uploads/2015/08/tobaccodisparity.pdf
Humphrey L, Deffebach M, Pappas M, Baumann C, et al. Screening for lung cancer with low-dose computed tomography: a systematic review to update the U.S. Preventive Services Task Force recommendation. Annals of Internal Medicine: 2013;159 (6):411-420.
Reck M, Heigener D, Mok T, Soria J, Rabe K Management of non-small cell lung cancer: recent developments. The Lancet 2013;382:709-719.
Richards T, Henley J, Puckett M, Weir H, Huang B, Tucker T, Allemani C Lung cancer survival in the United States by race and stage (2001-2009): findings from the CONCORD-2 study. Cancer 2017;123:5079-5099.
Zappa C, Mousa S Non-small cell lung cancer: current treatment and future advances. Translational Lung Cancer Research 2016;5(3):288-300.